
Caregiving through the Cancer Patient Journey
By Madan Jagasia, MD
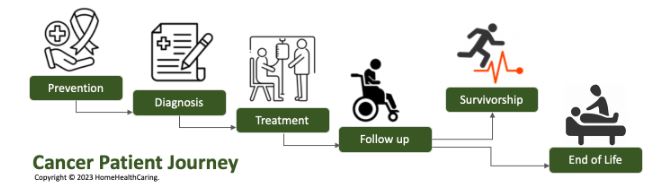
The journey of a cancer patient and their family caregivers is difficult and fraught with fear and anxiety. Caregivers are often tasked to make tough choices amidst uncertainty. The cancer control continuum framework has been used for the past 50 years to describe the various stages of the disease from cancer etiology to prevention, early detection, diagnosis, treatment, survivorship, and end of life. Understanding and using this framework to collaborate with your cancer care team will help you make better treatment choices, monitor progress, report on symptoms and side effects, and improve the patient’s overall quality of life. Not all cancers are the same and each patient’s journey is unique. Nevertheless, this framework will enable you to better care for your patient at home. Also refer to our Cancer Resources Library for more details on cancer care.
Prevention
The proven cancer prevention strategy currently include 5 main courses of action:
- Use of sun screens for prevention of Melanoma or skin cancers.
- Mammogram screening for early detection of breast cancer
- Pap smear for early detection of cervical cancer
- Colonoscopy for early detection/prevention of colorectal cancer
- PSA testing for early detection of prostate cancer (controversial)
All of the above have US Task Force Prevention (USPSTF), Centers for Disease Control (CDC), or respective professional societies’ guidelines. For example, the USPSTF recommends that women who are 50 to 74 years old and are at average risk for breast cancer, get a mammogram every two years. These guidelines across various agencies can be contradictory and confusing. The physicians often do not offer concrete guidelines. Consequently, patients tend to reach out to caregivers and their next of kin for advice.
Evolving paradigms in cancer prevention
Genetic tests are being done as part of diagnosis. The National Cancer Institute (NCI) suggests that 1 in 5 cancer cases may have a hereditary component. Thus, prevention based on genetics will continue to increase. As technology evolves, it may become confusing to interpret reports. Virus driven cancer is well recognized, especially from Human papillomaviruses (HPVs), and Hepatitis B virus (HBV), and Hepatitis C virus (HCV). Gardasil vaccine is expected to decrease incidence of cervical cancer in females, and incidence of oropharyngeal cancers of males and females.
Diagnosis
- Cancer diagnosis includes biopsy, pathology reports with genomics, and imaging (for staging). Other lab testing may be needed for diagnosis or to determine prognostic markers.
- It is very reasonable to get a second opinion for a cancer diagnosis. However, do not delay treatment for cancers that need emergent treatment.
- The American Cancer Society is an excellent starting point. Most academic centers and large community cancer centers have well developed online educational material. Patient advocacy groups are also good resources.
Treatment
As a caregiver or a patient, it is important to ask questions around:
- Expected efficacy of the treatment plan(s).
- Monitoring of disease, symptoms, and expected side effects.
- Medication management, as it is important to understand the effect and interactions of the cancer treatment and medications on current medicines for treating existing/other conditions.
- How to contact the health care team for routine, urgent, and emergent issues.
- Patient support needs and specific responsibilities for the caregiver.
- Ensure that the entire health care team including the primary care physician is aware and in the loop.As a caregiver, understand how you can help address the patient’s emotional needs.
Plan for logistical support for scheduling and transporting the patient for treatment and doctor visits etc., and have a backup if possible.
Discuss the patient’s nutrition and specific dietary needs with the care team incorporating cultural preferences, allergies, and any food restrictions. Managing the patient’s nutrition plan can become challenging if the patient lives in an area designated as a “food desert”.
Follow up
- Completing the initial treatment is a huge win. Cancer can leave a huge void and patients may struggle to readjust to normalcy. Celebrate the milestone!
- As a caregiver, understand the patient’s recovery goals with the care team.
- Ask about the follow up plan including oncology and primary care physician visits. Check on how often and why lab tests and imaging (x-Ray, MRI, CT Scans) may be needed.
- Discuss the potential interventions and treatment plans with the health care team if lab tests and/or imaging show a recurrence or a relapse. Keep a close watch in case symptoms reappear.
Survivorship
Survivorship intrinsically has psychological side effects for the patients and their loved ones. As a caregiver, be aware that patients:
- Struggle with how to live with remission and wonder if they will remain cured.
Worry about relapse. Does that translate into anxiety or depression?
Cope differently with the long-term physical consequences of treatments like chemotherapy, radiation, or undergoing transplant. - Survivorship is different from cancer follow-up where the focus is on treating cancer.
- Survivorship is thinking about the “whole” patient and includes vocational rehabilitation, and social rehabilitation, especially for young adults, as well as addressing any patient specific fertility, relationship, geriatric, or other related issues.
End of life
Patients and family members struggle with what might happen during the last stage of life. Understanding and planning for what to expect both physically and emotionally is important for both the patient and their family.
- When to stop treatment? When a patient’s care team determines that the cancer can no longer be controlled, medical testing and cancer treatment often stop. But the person’s care continues, with an emphasis on improving their quality of life and that of their loved ones and making them comfortable for the following weeks or months.
- Symptom control: Medicines at the end of life can control pain and other symptoms, such as constipation, nausea, and shortness of breath.
- A durable power of attorney/ advance directives: These legal documents should be ideally executed while the patient is still mentally aware and can make their wishes about receiving medical care known and/or give a person (such as a spouse, relative, or friend) the authority to make medical decisions on their behalf, when they are unable to do so themselves.
- Role of family and caregiver: Family and caregivers are affected by their loved one’s health more than they realize. Patient care causes physical and emotional fatigue, stress, depression, and anxiety. It’s important for caregivers to take care of their own bodies, minds, and spirits.
- Hospice: Hospice care offers many helpful services, including medical care, counseling, and respite care, and can improve the patient’s quality of life. Medicare states that hospice can be used as much as 6 months before death is anticipated when their doctor signs a statement saying that patients are unlikely to survive beyond 6 months.
- Preparing the family for the end: No one can fully predict what may happen at the end of life, how long the final stage of life will last, or when death will actually happen. Leaning in on the support of friends and family helps.
- Closure for the family: Closure can take a long time and every family’s circumstances are different. If you are having trouble managing your emotions, consider reaching out to your religious or spiritual mentors or asking healthcare providers for help or for a referral to a counselor or mental health specialist.

